You look at your life, and on the surface, you’ve done everything right. You’re the innovator, the high-performer, the ambitious student, the one who always excelled. You've built a career or a business on being capable, driven, and resilient.
Then, one day, you find you’re not.
The "simple" admin of life has become an impossible mountain. You’re missing deadlines, your emotional responses feel disproportionate, and your mind feels like a browser with 100 tabs open, all playing at once. You feel overwhelmed, anxious, or perhaps just... stuck. You look at your past success and your current struggle, and the two pictures just don't align.
This "crash" is often the first time a high-achieving adult truly meets their unmanaged Attention Deficit Hyperactivity Disorder (ADHD).
You’ve started researching, and for the first time, things are making sense. You're considering a private assessment to get clarity. But what happens after the diagnosis? What about medication? What about the cost?
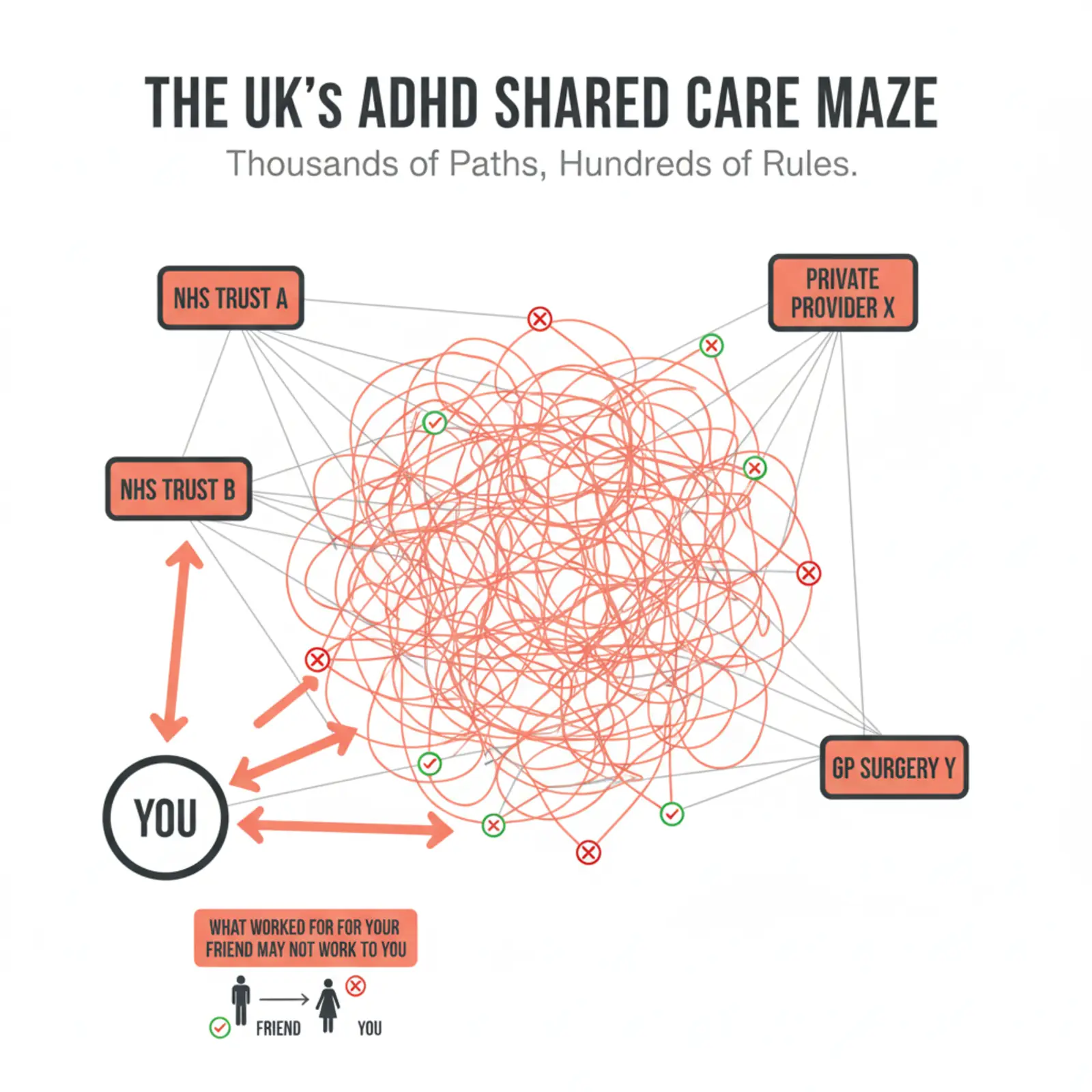
This is where you will meet one of the most complex and frustrating parts of the UK healthcare system: the ADHD Shared Care Agreement.
Understanding this before you start is the single most important strategic step you can take. It’s the difference between a seamless, sustainable treatment plan and a cycle of frustration, rejection, and wasted investment.
Today, we are going to explore this complex world. We will bypass the social media noise and provide a comprehensive, specialist-led view on what these agreements really are, why they are so often rejected, and a proactive strategy you can use to build a sustainable, long-term partnership for your care.
An Important Disclaimer
Before we begin, I must be very clear. This is a complex topic. The information in this article is for educational purposes only and does not, under any circumstances, constitute medical advice. It is based on the UK healthcare landscape, which can change rapidly.
Your individual situation is unique. You must always seek support and guidance from your own healthcare professionals (your GP and/or a specialist) before making any decisions.
Furthermore, the responsibilities detailed later in this article are provided as a general example to illustrate the complexity of these agreements. They are not our clinic's current set of responsibilities, and every single practice (both NHS and private) will have its own set of rules.
This guide is designed to give you the clarity to ask the right questions.

What is an ADHD Shared Care Agreement?
Many people think a Shared Care Agreement (SCA) is a simple form.
It is not.
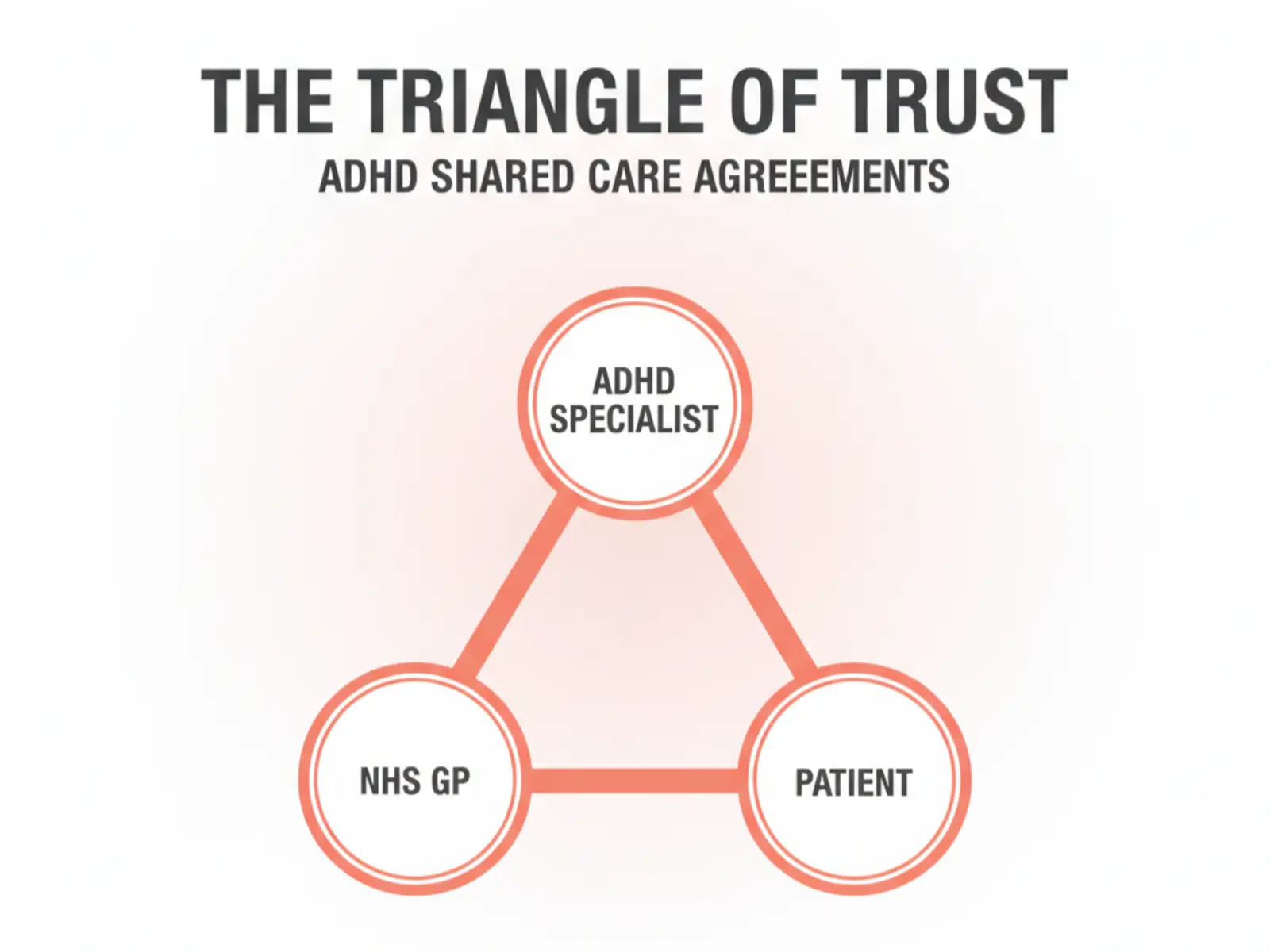
At its core, a Shared Care Agreement is a formal contract. It is an arrangement between three parties:
- Your ADHD Specialist (e.g., your private Consultant Psychiatrist or other healthcare clinician)
- Your NHS GP (Your Primary Care Partner)
- You, the Patient
Like any contract, it outlines a clear set of responsibilities for everyone. In this arrangement, the specialist initiates the diagnosis and "titration" (the clinical process of finding the right medication and dose). The GP then agrees to take over the "maintenance" part—primarily, writing the repeat prescriptions and monitoring your basic physical health (like blood pressure, heart rate and weight).
This sounds simple. But this is where the complexity begins. Many people assume there is one, single "Shared Care Agreement" form in the UK. This is incorrect.
The NHS is a vast organisation divided into different trusts. GP surgeries often run as independent businesses. There are now hundreds of private ADHD providers. This means there are potentially thousands of different versions, policies, and rules.
This is the first and most crucial thing to understand: what worked for your friend may not work for you. Their GP, their specialist, timing and their personal health profile are all different.
The "Admin Blindspot": Why Is This Process So Hard?
For a high-achieving professional, this process can be uniquely frustrating. You build businesses, lead teams, and manage complex projects. Why does a simple admin task feel so impossible?
This isn't a personal failing; it's often a direct symptom of the very condition you are seeking to treat.
Your brain is likely a "big picture" engine. You thrive on new ideas, solving complex problems, and high-stakes innovation. Your executive functions, however—the part of the brain that deals with mundane, detail-oriented admin, long-term planning, and following multi-step processes—may be your area of greatest challenge.
You are being asked to navigate a complex, bureaucratic contract… as a prerequisite for getting sustainable treatment for the very condition that makes navigating complex, bureaucratic contracts so difficult.
The irony is not lost on us. Understanding this "admin blindspot" is key to giving yourself the grace to ask for help, whether from a trusted person in your life or by ensuring you engage a professional service that handles this process with care.
Why You Must Understand This Before Your Assessment
A GP's refusal to sign an SCA often feels personal, but it’s almost always a decision based on professional risk management and resources. Your GP is being asked to take on the legal and medical responsibility for prescribing a "controlled drug"—a responsibility they do not take lightly.
Understanding the common reasons for rejection before you book an assessment is the most important part of your strategy. It allows you to vet your GP and your specialist to prevent a failed outcome.

Reason 1: The Trust Deficit (Patient Engagement)
This is a common concern for GPs. The SCA contract is clear: the patient must attend regular follow-up appointments with their specialist (usually every 6 or 12 months) for the agreement to remain valid.
The GP worries that a patient, once they have their "affordable" prescription, will disengage from the private specialist to save money. This leaves the GP alone, managing a specialist condition they are not trained for, with no expert support. This is a risk many are unwilling to take.
.webp)
Reason 2: The Provider Deficit (The Specialist's Credentials)
This is perhaps the most significant factor for a high-performing, discerning GP. Not all ADHD providers are created equal.
Given the substantial growth in new ADHD services, a GP's confidence in their specialist partner is paramount. They need to be assured that they are collaborating with an appropriately trained, robust, and professional service—one where they can readily access a clinical expert should you, the patient, experience any difficulties.
Your GP will ask:
- Who is this? Was it a Consultant Psychiatrist (a medical doctor on the GMC's Specialist Register) or another type of practitioner?
- How thorough was it? Was it a 15-minute checklist, or was it a multi-hour, comprehensive psychiatric evaluation that ruled out other conditions?
- Is this provider accessible? If the GP has a question, will they get a detailed, consultant-led response, or will they be lost in a generic admin email queue?
Choosing a high-quality, consultant-led clinic is your first and best strategy for reassuring your GP. You are, in effect, showing them that you are investing in a partner they can trust.
.webp)
Reason 3: The "Blanket" Rejection (Internal GP Policy)
This is the most frustrating, black-and-white reason. Some GP surgeries, or even entire Primary Care Networks (PCNs), have decided as a blanket policy that they will not accept any shared care agreements from any private provider, full stop.
Why? The reasons are often business-related, and it's important to understand the context. Over the past decade, GP budgets have been significantly stretched. This isn't a simple issue; it's a complex mix of rising patient caseloads, persistent staffing challenges, and the need to manage an ever-increasing number of complex conditions, all within a difficult funding environment.
Every prescription issued, every specialist letter read, every blood pressure check, and every second of a GP's time has a very real, unfunded cost. As official NHS England documentation on current GP contracts often illustrates, these practices operate under intense financial and operational pressures.
Faced with this, some practices have simply made the business decision that they no longer have the administrative or financial capacity to take on this extra, unfunded work.
.webp)
Reason 4: The Stability Requirement (The "Not Yet")
A GP most of the time is not an ADHD specialist. They are not comfortable managing the "titration" phase, where medication and dosages are being adjusted.
Many GPs will only accept an SCA once you are stable on a set treatment plan for at least 3 months.
This demonstrates that the initial "teething problems" are over, side effects are managed, and the specialist has found the optimal, effective dose. A rejection might just mean "not yet." The GP is waiting for the specialist to confirm, in writing, that you are stable and the plan is working.
.webp)
Reason 5: The "Out-of-License" Problem (Risk Management)
This is a major red flag for any prescriber. Most ADHD medications have a maximum licensed dose listed in the British National Formulary (BNF) and recommended by NICE (National Institute for Health and Care Excellence).
In some complex cases, a specialist may recommend a treatment plan that falls outside these standard guidelines (e.g., a medication that is used in other countries but not yet approved in the UK for ADHD, a combination of medications). While this may be clinically justified by the specialist, it places the GP in a difficult position. By prescribing "out-of-license," the GP is taking on a much higher level of personal medical risk. Many GPs will, understandably, refuse to do this.
.webp)
Reason 6: The "Whole Picture" Problem (Health Fluctuations)
An SCA is designed for a stable condition. If your mental or physical health is in flux, a GP will be hesitant.
If you have recently developed hypertension (high blood pressure), a new heart condition, or are struggling with co-morbid anxiety or depression, the GP will (rightly) feel that your case is not "stable." They will want the specialist to remain the primary clinician until your overall health picture is clear.
This comprehensive oversight is vital. We now have evidence that an ADHD diagnosis, with or without medication, can be linked to a potential reduction in life expectancy of up to 9 to 11 years, often due to these co-occurring physical and mental health conditions. This starkly illustrates why a GP will insist that your case is fully stable and well-managed by a specialist before they agree to take on prescribing.
.webp)
The Unseen Costs & The Human Element
It's easy to get frustrated about investing in private care when "the NHS is free." But this belief, while common, misses the unseen costs.
The NHS is funded by the taxpayer, but it runs on finite resources—human, financial, and infrastructural. Your GP's time, their nurse's time, the medication cost, the estates, insurance, the administrative support—it all has a very real cost.
This is also true for private services. In an industry like mental health, which is prone to professional burnout, sustainable, high-quality care requires significant investment. The best clinicians—the ones you want managing your health—must be supported by a robust infrastructure that allows them to provide safe, thorough, and unhurried care.
Healthcare professionals are human. We are all bound by the same pressures, stresses, and capacity limits. A successful Shared Care Agreement relies on a partnership where every party, including the professionals, feels supported, respected, and safe.

The Triangle of Responsibility: An Example
A successful SCA is built on a triangle of trust and not a drama triangle. For this to work, every person must understand and fulfil their specific obligations.
As we stated at the beginning, the following lists are a general example only. Every single practice has its own set of rules. These are not our clinic's specific responsibilities, but they are similar to what you might expect.
We have provided seven example responsibilities for each party to illustrate how the workload is shared.
Example: The Specialist's Responsibilities
(The expert who provides the diagnosis and treatment plan)
- Conduct a comprehensive diagnostic assessment, including psychiatric history, impact on functioning, and ruling out other conditions.
- Provide a detailed diagnosis report and care plan to both the patient and the GP.
- Establish a stable and effective treatment plan, discussing all benefits and side effects with the patient.
- Initially prescribe and titrate the medication, monitoring the patient's response and physical health (e.g., blood pressure, heart rate, weight) until stable.
- Communicate clearly with the GP, providing all necessary information for them to take over prescribing safely.
- Offer a mandatory annual (or 6-monthly) specialist review to monitor long-term efficacy, side effects, and the patient's overall mental health.
- Be accessible to the GP for advice and take back care if the patient's condition becomes unstable.
Example: The GP's Responsibilities
(The partner who provides ongoing prescribing)
- Formally accept or decline the Shared Care Agreement in a timely manner (e.g., within 3 weeks).
- If agreed, issue repeat prescriptions as recommended by the specialist.
- Facilitate the patient's physical health monitoring (e.g., blood pressure, pulse, weight) as per the agreement (e.g., every 6 months).
- Report any significant changes in the patient's physical or mental health (e.g., new heart conditions, severe anxiety) to the specialist.
- Check for drug interactions if any new medications are prescribed.
- Remind the patient of their obligation to attend their mandatory annual specialist review.
- Inform the specialist to take back prescribing if the patient does not engage in monitoring or if unmanageable problems arise.
Example: The Patient's Responsibilities
(The active partner who makes the agreement function)
- Attend your mandatory specialist review every 6 or 12 months, as set by your specialist. (Failure to do so is the most common reason for an SCA to be stopped).
- Arrange and attend all required physical health checks (e.g., blood pressure, weight) with your GP, pharmacy, or at home.
- Take your medication exactly as prescribed and do not change your dose without consulting your specialist.
- Report any side effects or changes in your mental or physical health to both your GP and your specialist.
- Do not use illicit substances, as these can be dangerous when combined with ADHD medication.
- Give both your GP and specialist permission to communicate with each other about your care.
- Understand that this is a long-term commitment and budget for any ongoing private costs (e.g., the annual specialist review).

A Proactive Strategy: How to "Start Well"
Now that you understand the complexity, the risks, and the responsibilities, you can move from a place of uncertainty to one of strategy.
Starting your ADHD care journey is one thing. Maintaining good, sustainable ADHD care is another. It is difficult, but not impossible.
Here is a clear, proactive 3-step plan to give you the best possible chance of success.
Step 1: Conduct Your GP "Due Diligence" (Before You Book)
This single step can save you thousands of pounds and immense frustration. Before you even choose a specialist, have a conversation with your GP surgery.
Speak to the Practice Manager and ask:
- "Does this practice have a policy on Shared Care Agreements for adult ADHD?"
- "Do you accept shared care from private providers?"
- "If so, do you have specific requirements for that provider?" (e.g., Must they be a Consultant Psychiatrist? Must they be on a specific register?)
Their answers will determine your next step. If they say "no" to all private care, you know you must either continue fully private or be prepared to change your GP surgery.
.webp)
Step 2: Vet Your Specialist (The Investment)
As we've discussed, your GP's trust in your specialist is paramount. You are not just buying a diagnosis; you are investing in a partner your GP will feel comfortable working with.
When researching clinics, ask them:
- "Who will be conducting my assessment? Is it a GMC-registered Consultant Psychiatrist?"
- "What does your assessment involve?" (You want to hear "comprehensive," "holistic," "rules out co-morbidities"—not "quick online test").
- "What are the ongoing costs to maintain this arrangement?" (e.g., the cost of the mandatory 6 or 12-month review).
- "What is your success rate with SCAs, and what happens if my GP rejects it?"
A good clinic will have clear, confident answers to all these questions.
.webp)
Step 3: Understand the Long-Term Commitment (The Strategy)
A Shared Care Agreement is not a "one-and-done." It is a long-term commitment. You must budget for the mandatory ongoing specialist reviews.
Think of it like owning a high-performance car. Your GP is the one who puts fuel in the tank (the prescription), but it must go back to the specialist dealership for a full service and diagnostic check-up (the follow-up) at least once a year. Trying to skip this annual service is what causes the entire arrangement to break down, and you must budget for the reality that, just like with a car, some years you may need more than a standard check-up. New issues might require extra visits, or in more complex situations, even a significant 'engine rebuild' to reassess your entire treatment plan.
.webp)
Conclusion: Beyond the Agreement – A Partnership for Life
A Shared Care Agreement is a complex, fragile, but powerful tool. It’s a contract, yes, but at its best, it's a partnership. It’s a commitment from three people to work together to manage a chronic, lifelong condition.
Its success depends on communication, trust, and a clear understanding of everyone's responsibilities—especially your own.
At our service, we have a very high success rate with Shared Care Agreements because we have built our entire model on the principles your GP is looking for: consultant-led, comprehensive care, clear communication, and a long-term, holistic partnership.
Of course, when an SCA is not accepted, we continue to support our patients with their needs fully in the private sector. But we believe in building bridges with the NHS wherever possible.
This journey requires investment—of your time, your finances, and your commitment. But the clarity and quality of life that come from a well-managed, sustainable treatment plan are invaluable.

ADHD Specialist Support: Assessment and Sustainable Care
Are you wondering if you might have adult ADHD? Our guide walks you step-by-step through the journey of a comprehensive diagnosis.
If you live in London or the UK and are looking for a private psychiatrist specialist in ADHD, we are here to support you.
Read more about our clinic's approach to diagnosis, treatment, and ongoing care or contact us to book your private assessment.
References
ADHD Diagnosis: More Than Just a Label
ADHD in Executives: Build Performance and Resilience
Struggling First Year Uni? Could It Be Undiagnosed ADHD?
ADHD and Career Burnout: Causes, Signs & Recovery Tips
Private ADHD Assessment London | Adults & Teens (16+) | UK
ADHD Specialist - Adult ADHD Symptoms & Diagnosis London & UK
ADHD Diagnosis: Likes, Swipes, and the Search for Clarity
NHS England » Implementing the 2025/26 GP Contract
Attention deficit hyperactivity disorder | Treatment summaries | BNF | NICE
Overview | Attention deficit hyperactivity disorder: diagnosis and management | Guidance | NICE
The NHS is not free — Adam Smith Institute
Trapped in the ADHD Drama Triangle? How to Break Free
ADHD: How to get an accurate diagnosis in UK?
Disclaimer: The information is not intended nor implied to be a substitute for professional medical advice, diagnosis or treatment. All content, and information, contained in this article is for general information purposes only and does not replace a consultation with your own doctor/health professional. Information about mental health topics and treatments can change rapidly and we cannot guarantee the content's currentness. For the most up-to-date information, please consult your doctor or qualified healthcare professional. For more information, you can check the Royal College of Psychiatrists (rcpsych.ac.uk)
Pictures source Pexels.com; Shutterstock.com Free Stock Photos, Royalty Free Stock Images & Copyright Free Pictures · Pexels ; Stock Images, Photos, Vectors, Video, and Music | Shutterstock
.svg)
.svg)





.svg)






